This will be the last entry in our series of optical instrumentation for optometry. If this is the first article that you are seeing, I would suggest that you take a look at our previous articles about Ophthalmoscope Design, Keratometer Design, and Retinoscopy. This week, we will talk about a very interesting optical device that uses the mechanical properties of the eye to make a measurement.
Internal ocular pressure is measured with non-contact tonometers, which aids in the diagnosis of glaucoma. The method of measurement is pretty intriguing. The patient is subjected to an air pulse that distorts the shape of his or her eye. The amount of distortion and the time it takes for the eye to return to its natural shape are then monitored using infrared light.
To fully comprehend this technology, we must first examine the biomechanics of the cornea. The cornea is depicted schematically in Figure 1.
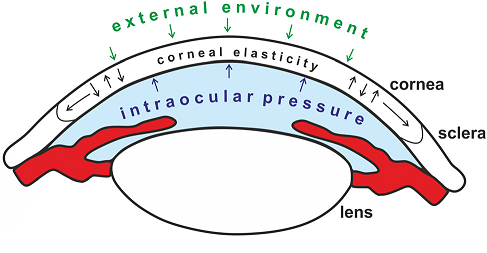
Figure 1. Schematic showing the different forces on the cornea. Image from P. Mlyniuk et al.
Many biological tissues, including the cornea, have viscoelastic qualities. That is, depending on the rate at which a force is delivered, it will react differently. The so-called Newtonian Fluids, which a person can walk over if they move quickly or sink if they travel slowly, are another viscoelastic material that many readers may be familiar with. The non-linear behavior of viscoelastic materials is an important factor to consider. When it comes to the cornea, The stress–strain curve can be broken down into sections to show changes in collagen organization during stress. The viscous reaction of ocular tissue is dominant at low distortion, whereas the elastic response is dominating at big deformation.
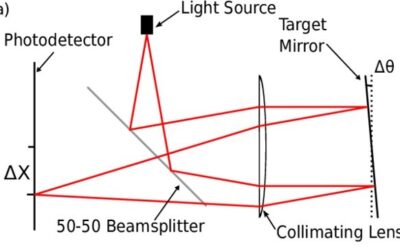
Due to copyright constraints, details on a commercial non-optical tonometer are difficult to come by. The fundamental layout of a non-contact tonometer is shown in Figure 2. As you may expect, we have two distinct systems. One is mechanical, which controls the puff of air, and the other is optical, which handles the measurements. We need to be able to manage the force and speed of air release for the air-puff, but we won’t discuss that mechanism here (this is an optic blog, after all).
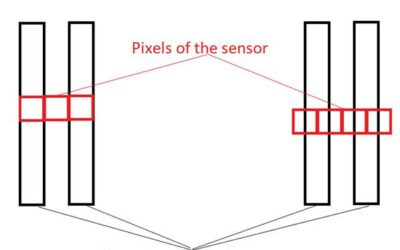
A light source (typically infrared/visible), image optics, a photodetector (PD), and a position sensing detector are among the optical components (PSD). The cornea is in what is known as a “applanation state” after the air puff has been released. The cornea’s front portion flattens out like a mirror, reflecting the maximum amount of light from the lightsource into the PD. This will be visible as a peak in reflection that gradually fades as the cornea returns to its original shape. The PSD was utilized to determine the corneal strain. To account for the image deformation caused by the light source and detectors being off-axis, we’ll require a cylindrical lens.
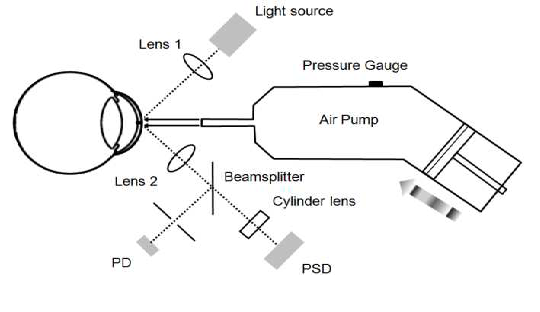
Figure 2. The non-contact tonometer configuration. A photodetector (PD) and a
Position sensing detector (PSD) are syed to monitor the status of cornea applanation and the
cornea displacement, respectively. Image after Wai W Wang et al.
Non-contact tonometers are widely used, although they are not the only method for measuring intraocular pressure. Commercially available methods include the Ocular Response Analyzer (ORA) and Corneal Visualization Scheimpflug Technology (Corvis CT). Because of its imaging speed, noncontact nature, and high image quality, optical coherence elastography (OCE) has a lot of clinical potential.